The Myth of a Medical Explanation for Vampirism
The problem is that real people suffer from these conditions.

The vampire myth has been around, in one form or another, for millennia. Tales of the undead with a penchant for sucking life from living were even told in ancient Egypt, long before Vlad III or Bram Stoker. The specifics of the legend vary in different parts of the world, but the core tale, involving blood-drinking revenants, comes up again and again. Modern scholars have looked to medical literature for an explanation of the universality of the myth, and in some cases suggested that what we know as vampirism is, in fact, based on the symptoms of known diseases. But connecting a feared mythical creature to a real human disease—and the real people who suffer from it—has consequences.
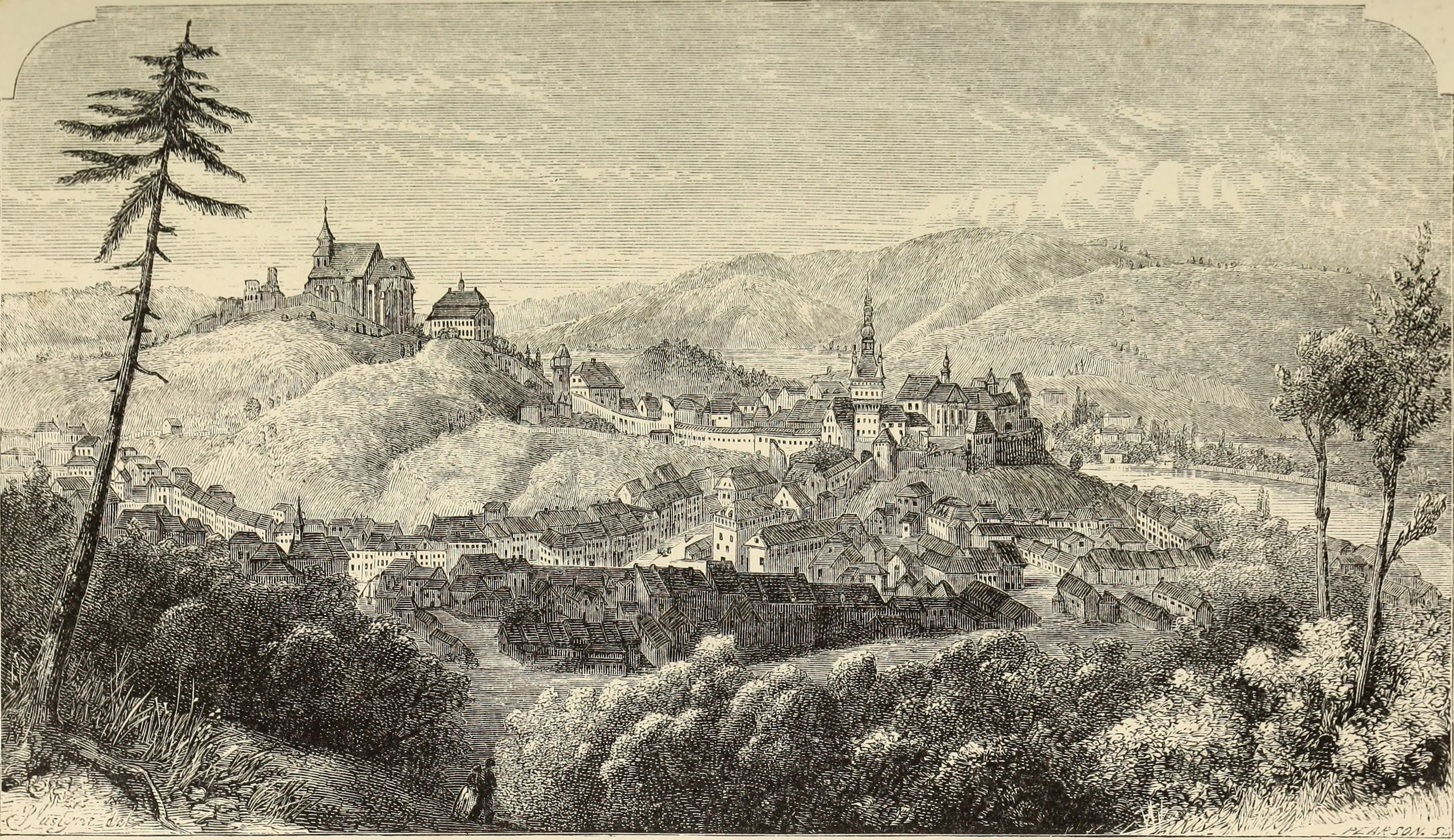
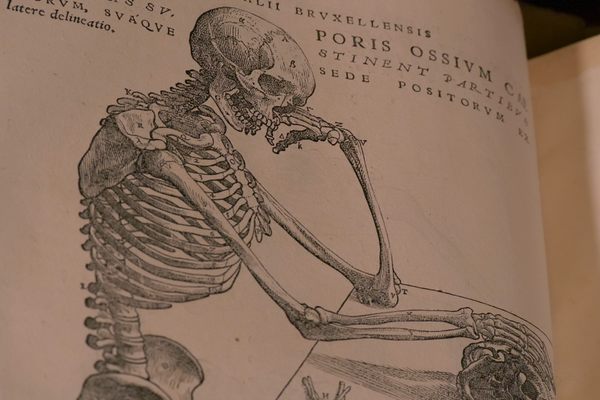
The most widely known vampire mythology today draws on Slavic folklore and stories from the 18th century. The stories tend to involve a recently deceased family member who, upon exhumation, didn’t seem to have decomposed at all, and instead appeared to be full of fresh blood. This was still the thinking in early-19th-century New England. Novels such as Carmilla (1871) and Dracula (1897) featured vampires that were mobile, rather underground undead. Eventually, light sensitivity and an aversion to garlic were added to the classic vampire folklore.
Connecting the many variations of the vampire myth to diseases that we now understand is a tall order, but people have tried. A 1998 article in the journal Neurology posits that rabies’s characteristic hallucinations and agitation are one source of the myth. Pellagra, a deficiency of niacin and tryptophan that causes sun-sensitive skin, a red tongue, and erratic behavior, has also been fingered as a culprit. Tuberculosis and schizophrenia, too.
In a talk at a conference in 1985, Canadian biochemist David H. Dolphin proposed that vampire and werewolf myths derived from a disease known as porphyria, the New York Times reported. The symptoms of congenital erythropoietic porphyria, in particular, were cited: light-sensitive skin, a lack of heme (a molecule in hemoglobin) that could have driven sufferers to bite others and drink blood, and sensitivity to garlic. It was not the first time Dolphin had suggested the link. He mentioned it in a 1982 speech to the Royal Society and again during a 1984 appearance on NBC.

No one apparently questioned the hypothesis at the conference, but it has since become the subject of plenty of contrary opinions. A 1995 article in Postgraduate Medical Journal, for example, questioned the evidence Dolphin presented, and noted that light sensitivity is a relatively modern addition to vampire lore, that people with the disease don’t crave blood, and that the disease is extremely rare. Perhaps the strongest condemnation of Dolphin’s idea was a 1990 article in Perspectives in Biology and Medicine. The authors, Mary G. Winkler and Karl E. Anderson, called Dolphin’s hypothesis a “medicalization of a myth.”
“There is a necessity for scientists and the media to set aside cynical assumptions about their audiences and consider first and foremost their responsibilities to the communities of patients who are affected by diseases and by stories about their diseases,” they wrote. They stated that despite critical comments from other doctors and scientists, Dolphin and the media continued to distort the public’s perception of rare diseases. That has translated to real effects on patients. One doctor, they wrote, “described a porphyria patient who was depressed and otherwise adversely affected by reports in the press linking porphyria and vampirism and required reassurance that he was not descended from vampires and would not turn into one.” Winkler and Anderson also cite the murder of a man in Virginia who claimed to have porphyria and thought he was a vampire.
Winkler and Anderson pointed out a critical flaw in the porphyria explanation. “Dolphin’s hypothesis assumes that vampires were real enough to require a medical explanation.” A medical explanation probably isn’t necessary at all—the myths could easily come from a misunderstanding of decomposition, or be the product of a generations-long game of “telephone” coupled with active imaginations.
“There will be a continuing need for the medical community to dispel this and other ill-founded notions that may link legends and myths to specific diseases,” they wrote. They advised doctors and scientists to avoid “interpreting mythology” as a topic for actual medical study or “allowing ancient, dark fears to dim scientific understanding.”
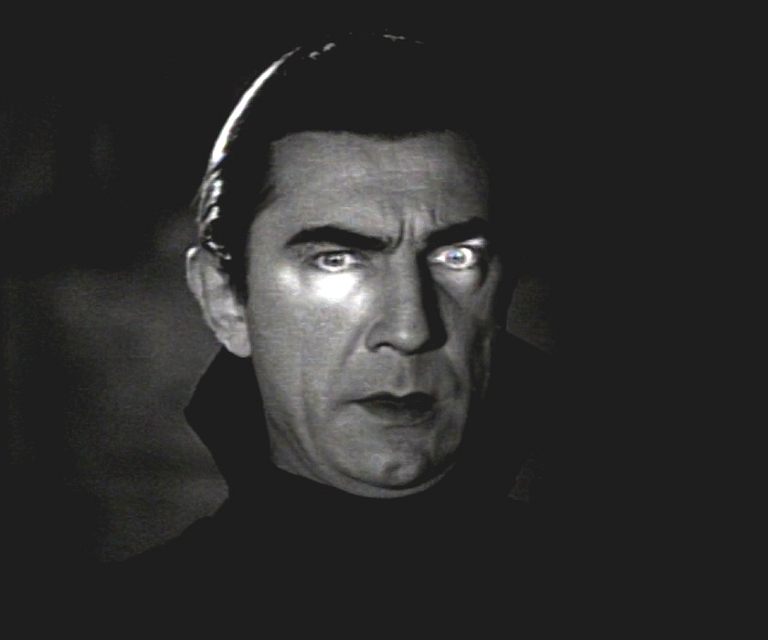
But their article certainly wasn’t the stake in the heart of the vampire-porphyria myth. Scholarly articles in well-known journals and press releases continue to link the genetic disease and the immortal mythical affliction, often around this time of year. Some have taken the message to heart, though. A 2016 article in JAMA Dermatology noted that, “Life with porphyria is difficult enough without everyone thinking you are Dracula.”






















Follow us on Twitter to get the latest on the world's hidden wonders.
Like us on Facebook to get the latest on the world's hidden wonders.
Follow us on Twitter Like us on Facebook